Because of health problems, A.C. Johnson has received aid from Centennial Hospice for the past year and a half. A couple of months ago, a wildfire destroyed the home he had lived in since the 1940s and everything in it. He almost lost his life, too, but his friend James Bradford realized he was still in the house and saved his life.
“I miss everything,” Johnson said. Since that ill-fated day, Johnson went to live with Bradford and receives at least weekly visits from hospice nurses, who have become more concerned and increased their visits.
“I think they are mostly worried about his condition: not his physical condition, but his living condition,” Bradford said.
The intent of hospice care is to keep patients comfortable toward the end of their lives, rather than focus on preventive care.
“We really make sure that our patients are out of pain, as much as we humanly can. (We) really just try to keep their dignity at the end of life,” said Katy Jump, executive director at Centennial Hospice.
Normally, patients stay in hospice care for about three months, until the end of their life. Jump called hospice care a “pre-paid service” because Medicare funds it, and sets the standards for who is eligible, based on the severity of a patient’s condition.
Medicare funds hospice care because it is considered a cost-saving measure: It can keep patients out of emergency rooms and hospitals because hospice nurses can determine if a patient is sick before conditions worsen.
“We’re trained professionals. We might see something before someone else might,” said Kathy Schumaker, one of Johnson’s nurses.
When she visits, Schumaker said she checks his vital signs, asks him how he’s feeling and makes sure he’s breathing normally. A lot of the care a patient receives is hygiene-related.
“We do a lot of upkeep,” Jump said. “Making sure they’re bathed and their nails are clipped, and that their hair is done and things like that, so that they still feel special and loved at the end of their life.”
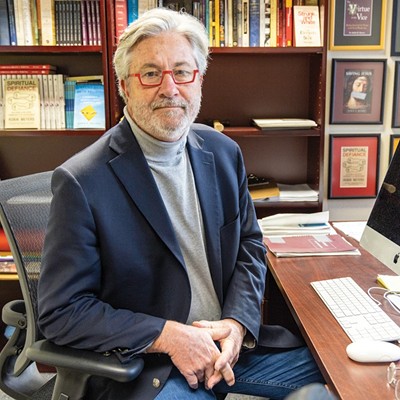
Photo by Mark Hancock